This time, the case details will be given in bits and pieces and not necessarily in order, just to make it interesting.
The scan revealed the following findings:
Cholelithiasis


Normal appearing liver and portal venous system.
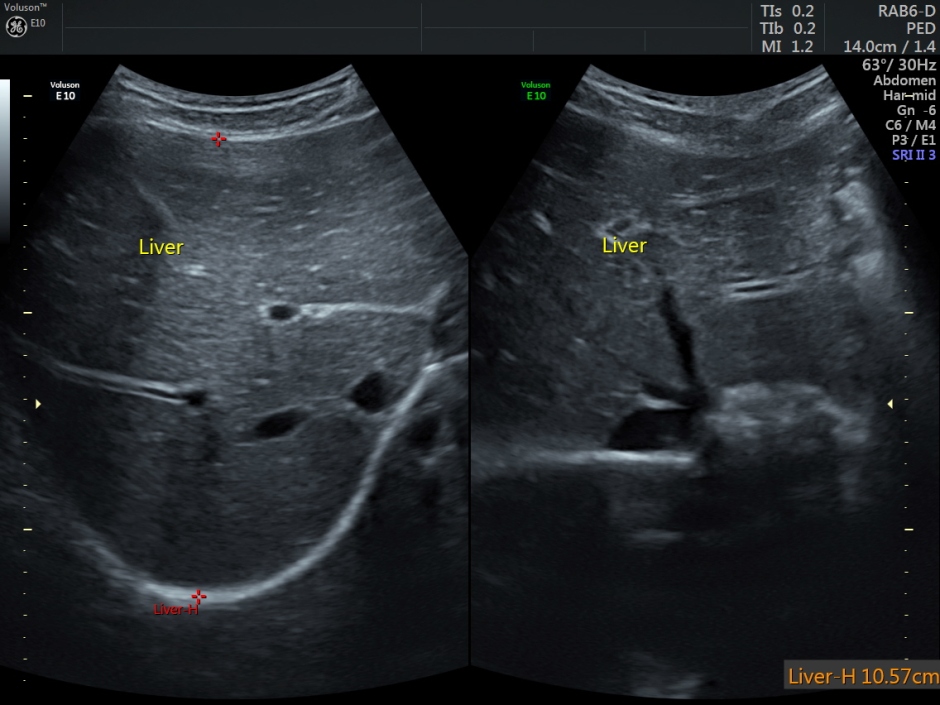

Mild splenomegaly

So what will be your diagnosis now?
I’m giving an important clue now – the age of the patient was 13 years.
I’m sure most of you have the diagnosis by now.
The child was being evaluated for persistent jaundice and anemia .
The serum total bilirubin was 10.97 mg/dl and the indirect bilirubin was 10.94.
The automated hemogram showed the following values:
Hemoglobin – 8.2 gms (low)
R.B.C. count 2.71 million/cu. mm (low)
PCV 22.6 ( low)
MC V 83.6 ( normal)
MCH 30.2 (normal)
MCHC 36.2 ( HIGH)
RDW 67.8 ( HIGH)
The diagnosis based on the findings available would be Hemolytic anemia with unconjugated hyperbilirubinemia and cholelithiasis.
An elevated MCHC would suggest Hereditary Spherocytosis.
In fact, this patient has been already worked up in a teaching institution many months ago. As she was advised splenectomy, the parents were afraid of any surgery and she was receiving some native treatment.The diagnosis was Hereditary Spherocytosis.
http://emedicine.medscape.com/article/206107-overview#showall
The following are excerpts from the above article.
Hereditary spherocytosis (HS) is a familial hemolytic disorder associated with a variety of mutations that lead to defects in red blood cell (RBC) membrane proteins. The morphologic hallmark of HS is the micro spherocyte, which is caused by loss of RBC membrane surface area and has abnormal osmotic fragility in vitro
The classic laboratory features of HS include the following:
-
Mild to moderate anemia
-
Reticulocytosis
-
Increased mean corpuscular hemoglobin concentration (MCHC)
-
Spherocytes on the peripheral blood smear
-
Hyperbilirubinemia
-
Abnormal results on the incubated osmotic fragility test
Standard blood studies for the workup of suspected hemolytic anemia include the following:
-
Complete blood cell count
-
Peripheral blood smear
-
Serum lactate dehydrogenase (LDH) study ( will be elevated)
-
Serum haptoglobin ( will be low)
-
Indirect bilirubin ( will be elevated)
Changes in the LDH and serum haptoglobin levels are the most sensitive general tests because the indirect bilirubin is not always increased.
Other laboratory studies may be directed by history, physical examination, peripheral smear, and other laboratory findings. Ultrasonography is used to estimate the spleen size since the physical examination occasionally does not detect significant splenomegaly. Chest radiography, electrocardiography (ECG), and other studies are used to evaluate cardiopulmonary status.
Splenectomy is the standard treatment for patients with clinically severe HS, but can be deferred safely in patients with mild uncomplicated HS (hemoglobin level >11 g/dL). Splenectomy usually results in full control of HS, except in the unusual autosomal recessive variant of the disorder.
Prophylactic folic acid is indicated because active hemolysis can consume folate and cause megaloblastosis.
Iron therapy is contraindicated in most cases of hemolytic anemia. The reason is that iron released from RBCs in most hemolytic anemias is reused and iron stores are not reduced.
However, iron therapy is indicated for patients with severe or intravascular hemolysis in which persistent hemoglobinuria has caused substantial iron loss. Before starting iron therapy, one should document iron deficiency by serum iron studies and, possibly, by assessing iron stores in bone marrow aspirates.

Spherocytes. One arrow points to a spherocyte; the other, to a normal RBC with central pallor

QUITE INFORMATIVE !
LikeLike
Thanks sir
LikeLike
WE FOUND A BOY OF 9YRS WITH GALLSTONE TREATED WITH SURGERY IN DINAZPUR, BANGLADESH.
LikeLike
WE ARE TREATING A GIRL OF 16YRS WHO HAD CLITOROMEGALY SINCE BIRTH AND HIRSUTISM RECENTLY
LikeLike
In case of splenomegaly radio-colloid isotope scan shows the site of red cell destruction
LikeLike
We are treating an obese boy of age 11 yrs with metformin, clomiphene and calcium to improve his hypogonadism. Please comment.
LikeLike
Is there any role of tamoxifen in hypogonadism?
LikeLike
We find concomitant DM and hypothyroidism improved by thyroxine and metformin
LikeLike
We postponed coronary angiography and pacemaker in pts.with DM,CKD, colonic polyps and Thyrotoxicosis
LikeLike
An obese girl of age 8yrs with body wt.40kg and pigmentations in the back of neck and both axillae, marked trunkal/central obesity was improved after metformin 250-500mg HS, ketoconazole 100mg daily, niacin 500mg weekly and dexamethasone test, being followed-up.
LikeLike